Why Generic AI Falls Short in Clinical Documentation
October 30, 2025
Why the Future of Smart Clinics Is Impossible Without AI Documentation
Smart clinics are revolutionizing healthcare with digital technologies, but medical documentation—the time-consuming recording of patient encounters—remains a major bottleneck. Physicians spend too many hours on EHR entries, reducing time for direct patient care. For example, one study found that for every eight hours a physician spends with patients, they spend over five hours interacting with the EHR (mostly documenting). This overload not only limits face-to-face patient time but is strongly linked to physician frustration and burnout. In response, AI-powered documentation tools are emerging to reduce administrative burden, a necessary step for “smart” clinics to achieve scale and productivity.
The Burden of Traditional Documentation
Accurate clinical documentation is vital, but traditional note-taking is inefficient and labor-intensive. Doctors spend the most time on documentation in the EHR, taking time away from patient interaction. This inefficiency often leads to after-hours charting (“pajama time”), contributing to burnout. Furthermore, manual documentation is prone to variability and human error. When rushed or fatigued, a clinician might omit important details or produce notes of inconsistent quality.
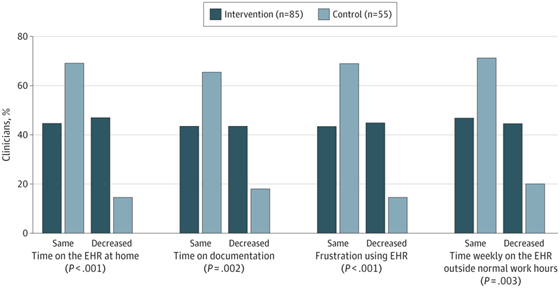
Figure 1: Survey results from a clinical trial of an AI-powered ambient documentation system. Many more clinicians with the AI assistant reported reductions in after-hours EHR time, post-visit documentation workload, and EHR-related frustration compared to those not using the AI. Automating real-time note-taking allowed physicians to reclaim personal time and feel less burdened by the EHR.
Relieving doctors of documentation duties also translates into greater efficiency. For example, using human scribes increased doctors’ weekly patient volume by about 6% while reducing the time they spent on documentation by roughly 9%. This demonstrates why smart clinics cannot scale without fixing the documentation bottleneck – when clinicians are freed from note-taking, they can see more patients or at least finish their workday on time.
Accuracy and Standardization Benefits of AI Documentation
AI documentation significantly boosts the accuracy and consistency of medical records by imposing a uniform structure, unlike varied human notes. AI medical scribes enforce standard formats (e.g., SOAP notes), automatically organizing key details from the conversation. This thorough, consistent approach saves provider editing time and improves care team communication by ensuring reliable, complete, and easily locatable patient information.
Patient Engagement and Time Allocation Improvements
AI-driven documentation significantly improves patient engagement. By having an AI scribe handle note-taking, doctors can focus fully on the patient, maintaining eye contact and listening actively, without the distraction of typing. This undivided attention makes patients feel more heard and satisfied, restoring the “human touch” to clinical encounters. This enhanced presence builds trust, improves communication, increases adherence to recommendations, and ultimately contributes to better clinical outcomes.
Privacy and Ethical Considerations
Integrating AI documentation requires robust privacy and ethical safeguards, including HIPAA compliance, encryption, and patient consent for recording conversations. Clinicians must, however, maintain responsibility for accuracy. Despite the high quality of AI-generated notes, errors like incorrect dosages or “hallucinations” can occur. Therefore, physicians must always review, verify, and correct the AI’s draft, remaining responsible for the final medical record content. This combination of AI efficiency and human oversight ensures accurate documentation and maintains patient trust.
Enabling Scalable and Efficient Clinic Operations
AI documentation is essential for a truly “smart” clinic’s scalability. Without it, expanding services means more clinician time on paperwork or costly staff additions like scribes. AI tools enable clinics to handle higher patient volumes without a proportional increase in administrative burden, freeing doctors to see more patients and boosting productivity without burnout. Integrating with existing EHRs, these tools ensure a consistent, scalable workflow across multiple sites. Essentially, AI-driven documentation lets clinics do more with the same resources, allowing growth without the bottleneck of manual charting—the core goal of a smart clinic.
TiM: A Case Example of AI-Driven Documentation
As a concrete example, consider TiM – an AI-powered clinical documentation assistant that illustrates the future of smart clinics. During a consultation, TiM listens to the dialogue between doctor and patient and generates a draft clinical note almost instantly. The physician then reviews and approves the note instead of writing it from scratch.
- Time savings: TiM instantly generates structured clinical notes from patient conversations, greatly reducing the time physicians spend on documentation.
- Hands-free documentation: Doctors have no need to type or dictate notes – TiM captures the details automatically while the physician focuses on the patient.
- Anywhere access: TiM is cloud-based, so clinicians can securely access notes anytime, anywhere, from any device.
- Data security: Patient privacy is paramount. TiM is built to comply with stringent standards like HIPAA and GDPR, ensuring data protection and confidentiality.
TiM shows how automating documentation makes clinicians more efficient and patient-focused. Such AI tools will likely be indispensable in the smart clinics of the future, enabling providers to be unburdened by paperwork and devote more energy to patient care while the documentation is handled intelligently in the background.